Clinical Governance For Nurses And Midwives Discussion
Introduction
Clinical governance refers to a set of relationships and roles put in place by a health service organization between its state or territory department of health, executive, governing body, patients, clinicians, and other participants to make sure there are good clinical results (ACSQHC, 2017a). Clinical Governance (CG) makes sure that the health service organization and the community can be assured that the systems have been established for the provision of secure and quality health care, and constantly improve services. Using the National Clinical Governance Framework and the ACSQHC CG for Nurses and Midwives documents as the primary references and supported by other scholarly sources, the essay will discuss elements such as the global, domestic, and local policy that influence CG in Australia, the clinical frameworks and practice standards, styles of leadership and management and their impact on CG, and how the culture of an organization affects the staffing, safety, and patient outcomes Clinical Governance For Nurses And Midwives Discussion.
ORDER YOUR PAPER HERE
Governance Structures in Australia
International, National, and Local Policy influencing Australia’s Clinical Governance
Halton et al. (2017) indicate that globally, CG policies and practices have been established to aid the delivery of safe and quality healthcare. The World Health Organization (WHO) for instance plays a vital part in governing health and diseases worldwide. WHO’s core governance roles are the establishment, monitoring, and enforcement of international standards and norms. WHO highlights the value of strong and receptive collective structures of governance in reinforcing worldwide nursing workforces and systems of healthcare (WHO, 2016)Clinical Governance For Nurses And Midwives Discussion. Liden (2014) indicates that WHO also coordinates the effective collaboration of its partners towards attaining the collective goal of safe and quality healthcare.
At the national level, there are various policies and standards that influence CG in Australia. These policies, legislations, and programs are developed by the federal Department of Health and they directly shape how healthcare services function (DoH, 2021). There is also the Australian Commission on Safety and Quality in Health Care (ACSQHC) which is the nationwide governing body whose function is to organize the enhancement of safe and quality care (Spigelman & Rendalls, 2015). The ACSQHC developed the National Safety and Quality Health Service Standards (NSQHSS) which is an influential healthcare standard with the objectives of improving the excellence of service delivery, enhancing patient results, safeguarding the citizenry from danger, and giving the people a nationwide unswerving proclamation on the degree of care they should anticipate from the professionals (ACSQHC, 2017b)Clinical Governance For Nurses And Midwives Discussion.
At the local level, the CG policies reflect the national policies but they are adapted to the situation, needs, and values of the local area. An example is the Western Australia Clinical Governance Framework developed by the WA DoH with the objectives of attaining safer, quality, culturally secure, and timely healthcare which is based on the values of WA Health (PSCQD, 2019). The ACSQHC guides that local health organizations like hospitals have the responsibility of developing procedures based on national and state policies and these should form the foundations of their procedures for reference by staff in their clinical practice (ACSQHC)Clinical Governance For Nurses And Midwives Discussion.
National Model Clinical Governance Framework
The National Model Clinical Governance Framework (NMCGF) was developed based on the NSQHSS, especially the standards on CG, and the partnering with consumers (ACSQHC, 2017c). The purpose of the framework is to make sure that patients get safe healthcare of high quality by defining the aspects that are vital for hospitals to attain embedded systems of corporate and clinical governance (ACSQHC, 2017c). The framework has five components as shown below: Clinical Governance For Nurses And Midwives Discussion
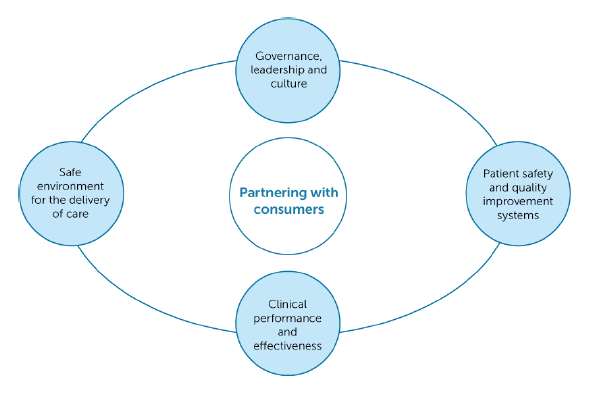
Fig 1: Components of the NMCGF
Clinical Frameworks and Clinical Practice Standards
Clinical frameworks are resource structures that guide the execution of clinical standards in the healthcare sector. In 2016, Australia established the National Model of Clinical Governance Framework (NMCGF) whose objective is to give the providers of healthcare the strategies for effecting the NSQHS standards. According to the ASCQHS (2017c), the NMCGF gives accountability to healthcare organizations in Australia that have to take on accreditation o prove their ability to apply the standards in practice. Another important framework is the NMBA’s Decision-Making Framework which was developed to guide the reasoning of the particular professional in delivering consistent and quality care (NMBA, 2020)Clinical Governance For Nurses And Midwives Discussion. The workplace injury-focused clinical framework for the delivery of health services is a non-discipline-specific framework developed by the Transport Accident Commission (2012) to provide the guiding principles for the delivery of healthcare.
Unlike the clinical frameworks which are principle-based, the clinical practice standards are inflexible statements of action against which care is measured. One example is the Registered Nurse Standards for Practice (NMBA, 2016) which specifies the standards that must be met by the registered nurses as dictated by the governing policies of the profession to promote the delivery of high-quality care. The clinical practice standards encompass 7 objectives based on care provision, engagement within the practice and application of quality, and safe critical thinking which meets the patients’ needs to promote quality outcomes (NMBA, 2020).
Leadership and Management Styles
Brown (2020) suggested that leadership determines the way of enacting CG and this has an influence on whether governance roles and responsibilities are addressed effectively. The ACSQHC (2017c) asserts that the role of a manager in CG is to advise and inform the corporate governance body and ensure that the systems established are properly designed and performed effectively. A leader may not have a designated formal duty but they emphasize people relationships, empower followers, and use their skills to impact optimal care delivery while managers have a selected formal managerial responsibility with authority and duties (Cope & Murray, 2017)Clinical Governance For Nurses And Midwives Discussion.
The most common styles of leadership in healthcare settings are transactional leadership and transformational leadership. Transformational leaders nurture collaboration and innovation by building respectful and trustworthy relationships and modeling the behavior that reflects the values and goals of the organization. Cope and Murray (2017) indicate that such leaders develop a robust culture of safety associated with accountability to CG structures and further related to quality enhancement instead of punitive reactions to adverse occurrences. Transactional leaders, on the other hand, depend on incentives and rewards to inspire commitment and performance, and Murray et al. (2020) claim that this style is not effective in quick-decision making and can nurture nursing care which is focused on tasks instead of holistic care.
Gauld and Horsburgh (2016) note that a positive connection between Nurse managers and the nurses strongly impacts the general execution and attainment of organizational goals, especially about CG. For instance, nurse managers who embrace a transformational leadership style will motivate their nurses by setting goals that are realistic hence motivating the nurses and creating a cohesive team culture.
Effect of Organizational Culture on Safety, Patients Outcomes, and Staffing
The ACSQHC (2017c) indicates that culture is significant in CG in making sure that patients and consumers get safe, quality health care. Day (2020) defined organizational culture as the collective beliefs, values, practices, attributes, and styles of communication that form expectations around the demeanor and social interactions of groups in a company. A good organizational culture is facilitated by safety, transparency and a blameless and constructive environment and its features include trustworthiness, openness, a willingness to share good practices, collaboration, support for patient safety, and learning from mistakes (Hershey, 2015)Clinical Governance For Nurses And Midwives Discussion. This type of culture minimizes errors, improves the safety and outcomes of patients, and enhances nurses’ job satisfaction leading to increased staff retention. In such a culture, clinical errors are approached as opportunities to learn and this culture also encourages adherence to the systems of reporting. Murray et al. (2020) assert that CG structures can depend on these reports to endorse productive quality enhancement initiatives that support the safety of patients as well as their positive outcomes.
Hershey (2015) notes that a poor organizational culture like the one which is reactive, unsupportive, distrusting, and punitive can result in lowered patient safety, undesirable outcomes, and insufficient staffing. A poor culture will lower the commitment of nurses and midwives to the hospital and intensify their job dissatisfaction and this leads to high staff turnover, poor retention of staff, and even some nurses quitting the profession for good. Work dissatisfaction and burnout among nurses are brought about by negative organizational cultures and surroundings and this results in increased attrition levels that hurt the safety and outcomes of patients (Murray et al., 2020)Clinical Governance For Nurses And Midwives Discussion.
The Role of the Registered Nurse/Midwife in Clinical Governance in Health Care Organizations
CG is a collective obligation to make sure that all patients are given the best care (ACSQHC, 2017a). Optimization of patient care is a common goal shared by nurses, midwives, and managers. The National Safety and Quality Health Service Standards (NSQHSS) indicate that the optimization of patient care necessitates that all nurses and midwives participate actively in safety processes (ACSQHC, 2017b). The ACSQHC outlines the roles of nurses and midwives for CG as follows: Clinical Governance For Nurses And Midwives Discussion
Governance, Leadership, and Culture
Nurses and midwives are expected to participate actively in developing a company culture that allows and gives priority to the safety and quality of patients (ACSQHC, 2017c). They should also communicate actively the commitment of the profession to deliver safe, quality health care. Nurses and midwives also have a responsibility to embrace opportunities to increase the knowledge of safety and quality systems and, to participate in all aspects of developing, executing, appraising, and monitoring the governance processes (ACSQHC, 2017a)Clinical Governance For Nurses And Midwives Discussion.
Patient Safety and Quality Systems
The ACSQHC indicates that nurses and midwives have a responsibility to make contributions in designing systems to deliver safe health care of high quality; give clinical care within these systems’ parameters; communicate both internally and externally with other clinicians to support quality clinical results; update their knowledge of safe system design, and adhere to the professional regulatory necessities and codes of conduct (ACSQHC, 2017c)Clinical Governance For Nurses And Midwives Discussion.
Clinical Performance and Effectiveness
The ACSQHC indicates that it is the responsibility of nurses and midwives to sustain individual professional abilities, expertise, and performance, make contributions to applicable company policies and processes adhere to the professional regulatory necessities, and code of conduct, and monitor their clinical output (ACSQHC, 2017c). They also have a responsibility to supervise and guide junior clinicians in their functions (ACSQHC, 2017a)Clinical Governance For Nurses And Midwives Discussion.
Safe Environment for the Delivery of Care
Nurses and midwives must make contributions to the preparation and improvement of activities that relate to the surroundings of the hospital, offer clinical care in the confines of these surroundings, be vigilant for opportunities to better the surroundings, and make sure that they appropriately raise and report the improvement opportunities identified (ACSQHC, 2017c)Clinical Governance For Nurses And Midwives Discussion.
Collaborating with Consumers
The ACSQHC indicates that nurses and midwives should comprehend the evidence on engagement with consumers and how it contributes to the quality and safety of healthcare. They should also have an understanding of the way health education can impact how a consumer accesses, comprehends and utilizes health knowledge (ACSQHC, 2017c). Further, nurses and midwives must collaborate with consumer representative associations to make sure that care systems are designed to help consumer engagement in making decisions (ACSQHC, 2017a)Clinical Governance For Nurses And Midwives Discussion.
ORDER HERE
Conclusion
The ACSQHS’s clinical governance for nurses and midwives document and the NMCGF have demonstrated that clinical governance makes sure that every person including nurses, managers, and boards, is responsible for the delivery of safe, quality, and effective health services to patients and the society. This discussion has established that hospitals are governed by CG structures which are influenced by global, national, and local policies, standards, and frameworks. The discussion has further highlighted how the culture of the organization impacts staffing and patient safety and outcomes. Lastly, it has been established that registered nurses and midwives have various roles in CG in hospitals based on the five components of the NMCGF Clinical Governance For Nurses And Midwives Discussion