The Report For Nursing Of Patients With Diabetes Mellitus
Diabetes is a debilitating condition which affects millions of people every year. It is evident from several research papers that type 1 diabetes is highly prevalent in patients with Down syndrome (DS). Diabetes present together with Down syndrome and moderate intellectual disability, it is very challenging to manage the complexities of diabetes. In Australia there are more than 13000 people with DS (O’Leary et al., 2013). According to the ABS Australian Heath Survey, there were 2,509 new cases of type 1 diabetes in Australia in the year 2014 (Wilkinson et al., 2014)The Report For Nursing Of Patients With Diabetes Mellitus. The essay deals with health challenges in a 45 years old man’s life span as the result of his Down syndrome, moderate intellectual disability, and Type 1 diabetes. The essay will discuss the impact of this health challenges on his physical and mental well-being. Using “International Classification of Functioning, Disability, and Health” ICF model the essay discusses how the presence of chronic illness and disability potentially affects the patient’s activity and participation. Lastly, it will identify one intervention for managing type 1 diabetes mellitus by performing a thorough literature review The Report For Nursing Of Patients With Diabetes Mellitus.
ORDER YOUR PAPER HERE
Down syndrome is a genetic disorder caused by “nondisjunction” during cell division. It results in three copies of chromosome 21 a condition also called trisomy (Glasson et al., 2014). The phenotypic features of people with Down syndrome include a flat face, small mouth, short neck, arms and legs, small ears, and slanting eyes. These patients have low intelligence which poses challenges in daily life functioning (O’Leary et al., 2013). The man in the case study is highly susceptible to mental retardation owing to his age. According to Mårild et al., (2013), DS patients have 70% chances of developing dementia at the age of 50. Down syndrome is associated with several comorbidities such as Alzheimer’s disease, congenital heart defects, gastrointestinal problems, hypertension and unique spectrum of malignancies such as leukemia (Glasson et al., 2014). The man in the case study is also associated with type 1 diabetes. In this condition, the body fails to produce insulin due to autoimmune destruction of pancreatic beta cells. It results in high blood glucose level and ketoacidosis due to unusual fat burn. The symptoms of type 1 diabetes include, excess weight loss, polyuria, unusual thirst, prone to multiple infection, muscle cramps, blurred vision and slow healing of wounds (Wong-Rieger & Rieger, 2013). They have the high risk of heart stroke, osteoporosis, thyroid, sexual dysfunction, kidney failure, neuropathy, skin disease and foot ulcer (Chiang et al., 2014)The Report For Nursing Of Patients With Diabetes Mellitus. These factors make the management of the chronic illness more complex and challenging and increase the likelihood of poorer health outcomes. Patient with a presence of DS and diabetes have a significant effect on mental health and social well-being due to dual challenges. Intellectual disability prevents them from engaging in health-promoting activities. They fail to adhere to medication therapy, sustain dietary restrictions, recognize early symptoms, manage weight and seek medical attention. (Haas et al., 2013) highlighted that depression, conduct disorder, and obsessive compulsion disorder is highly prominent in patients with chronic illnesses. Thus a targeted strategy is essential to support their habilitation at home and involve them in health promoting activities The Report For Nursing Of Patients With Diabetes Mellitus.
The ICF is a framework of World Health Organization (WHO), which helps to obtain organized information on functioning and disability based on the principles of primary health. It is essential for health and well-being of such patient. The framework determines an impact of the interaction of health and disability in an individual (Selb et al., 2015). The three core domains of this framework to determine the level of disability are “functional impairment, activity limitation, and participation restrictions.” It also includes activity and participation which relates to communication skills, mobility, and awareness about disease, self-care and others (Müller, 2014). As evident from the case study, this man is still physically active as he regularly attends and participates in the disability program five days a week. He is satisfied with the staff workers. The community programs are targeted to increase self-care in patients. Their primary goal is to support and help an individual develop the potential to participate in all the domains of life (Taggart et al., 2013)The Report For Nursing Of Patients With Diabetes Mellitus. Care providers face challenges in teaching the patient to deal with functional impairment. Since he has the moderate intellectual disability, it is not feasible for him to perform daily activities related to shopping, billing, and budgetary management. His cognitive impairment hampers his problem solving skills. It is also challenging for him to adhere to medication management, diet restriction, and weight management. The combination of these factors has limited his social and physical activity which exacerbated his disability. These factors have constrained his ability to participate in health affirming activities.
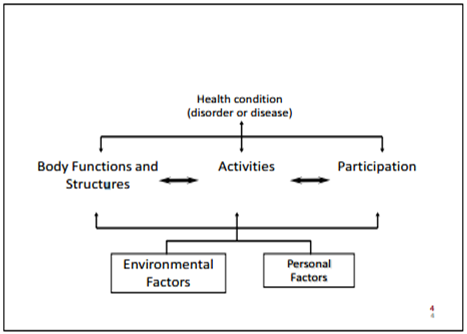
Figure: ICF model
Source: (Wong-Rieger & Rieger, 2013)
To address health needs of the man in the case study and to make the medical adjustment, it is necessary to view his needs from the perspective of the current standard of care and management. The caregivers must be well informed of the man’s health, and well-being is entirely dependent on their knowledge and perception. Insulin therapy is essential for treating type diabetes mellitus and control blood glucose level in the man (American Diabetes Association 2013). The insulin intake can be through injection or oral method. Oral medication for type 1 diabetes include pramlintide to minimize blood sugar rise, and angiotensin-converting enzyme (ACE) inhibitors to control blood pressure and cholesterol lowering drugs (Chiang et al., 2014)The Report For Nursing Of Patients With Diabetes Mellitus. It is necessary to monitor that the man adheres to this medication. (Ly et al., 2013) recommends that care management for type 1 diabetes should primarily include insulin intake, regular exercise, low carbohydrates, regular monitoring of BSL, and maintenance of healthy weight. It is recommended by the American Diabetes Association that blood sugar level (BSL) monitoring is critical for the patient of diabetes (Haas et al., 2013)The Report For Nursing Of Patients With Diabetes Mellitus. The blood sugar level before meals should be between 70 and 130 mg/dL and after meal numbers should not exceed 180 mg/dL. As a nurse, I would implement this intervention strategy for the man in the case study.
It is evident from the research paper American Diabetes Association, (2013) that helping patients to develop goods communication, and social skills will assist in carrying independent activities. I will use a holistic and Person-centered care to manage chronic illness and associated disability in the man. It is evident from the research paper (Wong-Rieger & Rieger, 2013), patients fighting with chronic illness and disability needs person centered care for effective outcomes. Referral services such as arranging for the psychologist, physiotherapist, dietician, the social worker is necessary for effective management of chronic illness (Wilkinson et al., 2015). It will help the man in addressing his physical, mental health issues. It will also assist in decreasing the comorbidities. The primary goal is to teach man about the self-monitoring of glucose. I would educate the man in a simple language about the consequences of nonadherence to medications, balanced diet, and weight management. At every visit, I would reinforce the information by repeating the relevant points. It is necessary because his cognitive impairment will disturb him in retaining information. Also well-informed patients highly participate in self-care activities. I would develop a routine for proper scheduling of eye check up and physical exam, exercises, walking, diet plan, and glucose monitoring. On a timely basis, I would evaluate the changes in the man. Since he is central to the success of the intervention program, I will include him in every decision. The strategies that I am going to use are highly likely to evoke positive health outcomes since they are based on the research evidence.
ORDER HERE
Conclusively, nurses can provide effective care only when they have adequate knowledge of the interaction of the chronic illness and disability. Understanding of the relationship between the functional impairment, activity limitation and participation restriction is essential to provide care for the chronic condition. It will enhance the effectiveness of the care practices adopted. The Report For Nursing Of Patients With Diabetes Mellitus